Lyme Disease
Lyme in Animals FAQ
District Tick & Lyme Activity
The District provides guidelines for how to prevent tick-borne diseases:
Reduce your chances of contracting tick-borne diseases by removing a tick promptly:
What Is Lyme Disease?
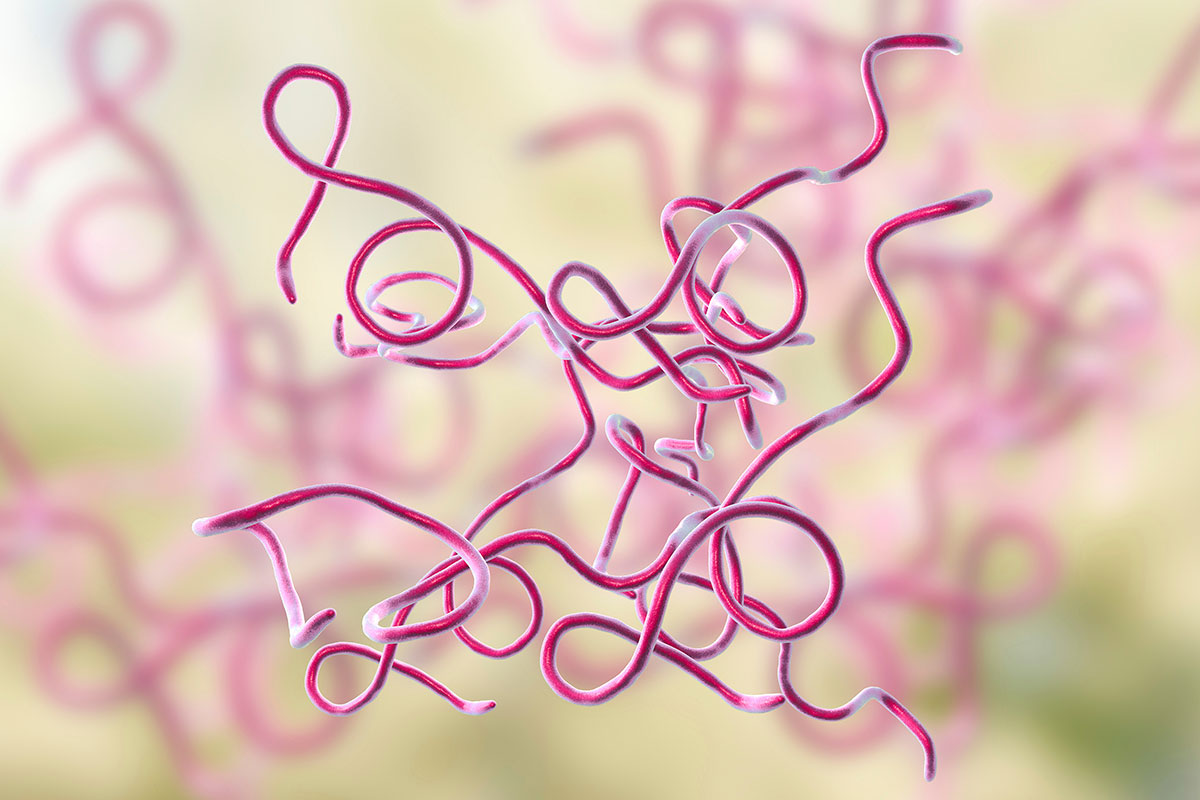
Lyme disease is an infection caused by the corkscrew-shaped bacteria Borrelia burgdorferi that is transmitted by the bite of deer (Ixodes scapularis) and western black-legged (Ixodes pacificus) ticks.
The deer tick, which normally feeds on the white-footed mouse, the white-tailed deer, other mammals, and birds, is responsible for transmitting Lyme disease bacteria to humans in the northeastern and north-central United States. On the Pacific Coast, the bacteria are transmitted to humans by the western black-legged tick.
The western black-legged tick is much smaller than common dog and cattle ticks. In their larval and nymphal stages, they are no bigger than a pinhead. Adult ticks are slightly larger. Larvae and nymphs take in spirochetes as they feed on infected mice. Infected larvae molt to infected nymphs and infected nymphs molt to infected adults.

How Does Infection Occur?

More cases of people infected with Lyme disease are the result of the feeding of infected nymphs rather than infected adults. Ticks will attach anywhere on the body, but prefer body creases such as the armpit, groin, back of the knee, and nape of the neck.
Most cases of Lyme disease occur between late spring and early fall when people are outdoors and ticks are most active. Ticks feed on blood by inserting their mouth parts (not their whole bodies) into the skin of a host animal. They are slow feeders: a complete blood meal can take several days. As they feed, their bodies slowly enlarge.
Who Is at Risk for Infection?
In the United States, the disease is mostly localized to states in the northeastern, mid-Atlantic, and upper north-central regions, and to several counties in northwestern California.
The number of annually reported cases of Lyme disease in the United States has increased about 25-fold since national surveillance began in 1982, and a mean of approximately 12,500 cases annually were reported by states to the Centers for Disease Control and Prevention (CDC) from 1993-1997.
Most B. burgdorferi infections are thought to result from exposure to infected ticks during property maintenance, recreation, and leisure activities. Thus, individuals who live or work in residential areas surrounded by woods or overgrown brush infested by vector ticks are at risk of getting Lyme disease.
When Do Symptoms Develop?
A red rash usually appears an average of 1 to 2 weeks after disease transmission. The early symptoms of Lyme Disease can be mild and easily overlooked. Although a majority of the infected develop the classic red rash, many do not.
People who are aware of the risk of Lyme Disease in their communities and who don’t ignore the sometimes subtle early symptoms are most likely to seek medical attention and treatment early enough to be assured of a full recovery.

What Are the Symptoms?
Early Symptoms
The first symptom is usually an expanding rash called erythema migrans, or EM, in medical terms. It is thought to occur in only about 50-60% of all Lyme Disease cases, and is characterized by the following:
- Usually (but not always) radiates from the site of the bite
- Appears a solid red expanding rash or blotch, or a central spot surrounded by clear skin that is ringed by a red rash (bullseye).
- Average diameter of 5″ to 6″
- Persists for about 3 to 5 weeks
- May or may not be warm to the touch
- Is usually painful or itchy
EM rashes appearing on brown-skinned or sun-tanned patients may be more difficult to identify because of decreased contrast between darker skin tones and the red rash. A dark, bruise-like appearance is more common on dark-skinned patients.
Around the time the rash appears, other symptoms such as joint pains, chills, fever, and fatigue are common, but they may not seem serious enough to require medical attention. These symptoms may be brief, only to recur as a broader spectrum of symptoms as the disease progresses.
Disease Progression
As the Lyme Disease spirochete continues disseminating through the body, a number of other symptoms can occur, including:
- Severe fatique
- Stiff, aching neck
- Tingling or numbness in the extremities
- Facial palsy (paralysis)
Later-Stage
The more severe, potentially debilitating symptoms of later-stage Lyme Disease may occur weeks, months, or, in a few cases, years after a tick bite. These can include:
- Severe headaches
- Painful arthritis and swelling of joints
- Cardiac abnormalities, and central nervous system involvement leading to cognitive disorders.
How Is It Diagnosed?
There is no test that can determine if a patient is infected with the Lyme Disease bacterium and then demonstrate that the patient has become bacterium-free.
Therefore, Lyme Disease is a clinical diagnosis based on signs and symptoms, with the patients travel history to endemic areas and test results being additional pieces of information in the complete picture. No test can “rule-out” Lyme Disease.
Certain tests, both indirect and direct, can aid in a proper diagnosis.
Indirect (Antibody) Tests
Antibodies are the immune system’s response to combat infection. Tests strive to be both sensitive (detecting any Lyme Disease antibodies) and specific (detecting just Lyme Disease antibodies).
Test Interpretation
- False negative tests occur due to defects in test sensitivity; too low an antibody level to detect (e.g. they are bound to the bacteria, with too few free-floating; the patient taking antibiotics or other drugs; naturally low antibody production); the bacterium has changed, limiting recognition by the immune system; or bacterial strain variations.
- False positive tests occur due to test failure or cross-reacting antibodies (e.g. syphilis, periodontal disease, ANA or RF).
Types of Tests
- Titer (ELISA, EIA, IFA) tests measure the level of Bb antibodies in fluid, with labs using different detection criteria, cut-off points, types of measurements, and reagents.
- Western blot tests produce bands indicating the immune system’s reactivity to Bb, with labs differing in their interpretation and reporting of these bands.
Direct Dectection Tests
Antigen Detection
These tests detect a unique Bb protein in fluid (e.g. urine) of patients. This may be useful for detecting LD in patients taking antibiotics or during symptom flare-up.
Polymerase Chain Reaction (PCR)
This test multiplies the number of Bb DNA to a detectable measurable level.
Culturing
Growing the bacterium in culture is difficult and can take months.
Staining
Staining of tissue is time consuming and has low yield. The problem is that in Lyme Disease there are too few of the Lyme spirochete in the body, and could result in the biopsy having no bacteria.
How Is It Treated?

No definitive treatment regimens have been determined, and failures occur with all protocols.
- Oral antibiotics may be sufficient for early stages of non-disseminated infection.
- Long-standing or Disseminated Lyme Disease responds best to one or several courses of either oral or intravenous antibiotics.
- Physicians and researchers agree that it is unethical not to treat people with demonstrated, persisting infection, therefore, some people receive retreatment or longer treatment.
How Is Lyme Identified in Animals?

Lyme disease can affect individual animals differently. Some may display no symptoms. Others may develop fever, loss of appetite, painful joints, lethargy, and vomiting.
If left untreated, the spirochete may damage the eyes, heart, kidneys, and nervous system. Lyme disease has been diagnosed in humans, dogs, cats, horses, goats, and cattle. Other species may also be at risk.
Cats
Cats may show lameness, fever, loss of appetite, fatigue, eye damage, unusual breathing, or heart involvement. Many cats do not show noticeable symptoms, despite being infected.
Dogs
Infected dogs may be lethargic, have a poor/loss of appetite, or a fever (103° – 105 ° F). Dogs may also experience lameness shifting from one joint to another, fatigue, kidney damage or failure, heart disorders, or neurologic involvement (e.g. aggression, confusion, overeating, seizures). Dogs can be infected with the Lyme bacterium but not exhibit any noticeable symptoms. Dogs appear to have the same expression of disease as humans, therefore, humans have been considered an animal model for dogs. Transplacental transmission has occurred in dogs.
Cattle
Many cattle do not display signs of Lyme Disease; those that do may have lameness, painful or swollen joints, fever, laminitis, or weight loss. A skin rash may be present on the udder of infected cows. Bb has been found to exist in urine and colostrum of infected cattle; therefore, the possibility of transmission between cows should be considered. The Lyme bacterium has also been found in blood, milk, synovial fluid, and spontaneously aborted fetal tissue. Bb can survive in frozen milk, but is killed during pasteurization.
Horses
Infected horses generally do not have a fever, but may have lame or stiff joints, laminitis, depression, or refuse to eat. This bacterial infection may be a cause of moon blindness or loss of vision. There have been reports of spontaneous abortion and encephalitis in horses infected with Bb. Neurologic signs include head tilt, difficulty swallowing, or aimless wandering. Trans-placental transmission occurs. Colts born to infected mares have displayed birth defects. Many horses may be infected with the spirochete, but display no symptoms.
How Can I Protect My Pet?

Vaccines are available for dogs.
Take precautions to guard against ticks when entering tick habitat, such as grassy, shrubby, wooded, or beach grass areas.
Cut down or mow grassy areas regularly to reduce tick habitation. Treat the environment with insecticides designed specifically for ticks. To avoid contaminating water, experts recommend spraying at least 75 feet away from a well.
Tick Checks & Removal
Conduct frequent tick checks. Examine animals closely in order to detect embedded ticks.
Tick Removal
- Remove attached ticks properly and promptly to reduce the chance of transmission of the Lyme bacterium.
- Place fine point tweezers around the tick’s mouthparts (the place where the tick is attached) and gently pull upwards until the tick detaches.
- Do not use your bare fingers!
- Disinfect the bite site and tweezers after removal.
- Wash your hands.
- Place the tick, along with several blades of grass, into a small container (e.g. a clean screw-cap pill bottle or a zip-lock bag) for later examination.
- Label the container with: the date, name of pet, type of animal, owner’s name, address and phone number.
- Call your veterinarian to determine if there is a local place where the tick can be tested.
- Have your animal(s) examined as soon as possible if you notice any symptoms of disease; the sooner a disease is diagnosed, the easier it is to treat.
Tick-Killing Chemicals
Apply tick-killing chemicals to your animals in order to protect them from disease spreading ticks.
- Sprays and dips containing permethrins and pyrethrins kill ticks on dogs, cats, and horses.
- Precautions should be taken when applying insecticides as some animals may be sensitive to the chemicals
- Follow the manufacturer’s application instructions.
- It is a good idea to wear rubber gloves during application.
- Tick collars will help discourage ticks from attaching to your pet(s).
- Never apply multiple repellents on your pet as a mixture of different chemicals could make the animal very sick.